Hyperadrenocorticism (Cushing's syndrome) is a rare disease in cats. It develops when there is persistent overproduction of the hormone cortisol by the adrenal glands, or the body receives it orally, topically, or by injection. Excessive cortisol concentrations lead to various abnormalities, including aggressiveness, weakness, and skin changes. Although hyperadrenocorticism is less common in cats than in dogs, it is more difficult to treat, but successful treatment is still possible. Middle-aged and elderly cats are most often affected.
Symptoms
The symptoms accompanying Cushing's syndrome are nonspecific. Only a specialist can refute/confirm the pathology by comprehensively considering the existing symptoms.
Itsenko-Cushing may be accompanied by symptoms such as:
- Obesity. This is the main symptom of the pathology. Local obesity - in the abdomen, face, neck, back. The legs remain thin.
- The face is round and bluish. Dark red in places.
- Muscle thinning, hypotonicity.
- The skin gets a specific marble shade. The appearance of stretch marks, a clear vascular network, desquamation, and dryness is noted.
- Very thin, almost transparent skin on the back of the hand.
- Osteoporosis, kyphoscoliosis/scoliosis.
- Cardiomyopathy.
- Dysfunction of the central nervous system.
- Diabetes mellitus (steroid form).
- Hyperandrogenism (typically female symptom).
With Itsenko-Cushing, complaints of general weakness and headaches appear.
Causes of Cushing's syndrome in cats
There are three causes of Cushing's syndrome:
- Iatrogenic (veterinary induced/caused). It results from excessive amounts of corticosteroids (especially cortisol) taken into the body orally, topically, or by injection.
- Hyperadenocorticism due to adrenal disease. Typically, this form of the disease is a consequence of a tumor of the adrenal cortex, which causes an overproduction of glucocorticoids. One or both of the adrenal glands ignore the signal from the hormone ACTH and begin to produce excessive amounts of corticosteroids. Typically, this is the result of a benign or malignant tumor. Approximately 50% of adrenal tumors are cancerous.
- Pituitary hyperadenocorticism – PDH (pituitary disease). Microtumors in the pituitary gland can lead to the production of excessive amounts of adrenocorticotropic hormone (ACTH). ACTH stimulates the adrenal glands and they produce too much cortisol.
Treatment
The goal is to bring the level of hormones of the adrenal cortex to the physiological norm.
Drug treatment
Drug treatment is symptomatic therapy. To relieve symptoms, the following groups of medications are prescribed:
- antihypertensive;
- sugar-lowering;
- diuretics;
- cardiac glycosides;
- immunomodulators;
- antidepressants;
- sedatives;
- vitamins.
Osteoporosis therapy is being carried out.
Surgery
Surgical treatment of pathology is carried out in the presence of hormonally active tumors. The following methods are implemented:
- bilateral adrenalectomy;
- selective transsphenoidal adenomectomy;
- abdominal surgery;
- destruction of the adrenal glands.
Radiation and proton therapy for Itsenko-Cushing syndrome is carried out according to indications.
Alternative Treatments
The clinical protocol is allowed to be supplemented with secondary methods.
Nutrition
In case of Itsenko-Cushing syndrome, it is necessary to reconsider nutrition. The following must be excluded from the menu:
- foods with saturated fatty acids;
- strong tea/coffee, any alcohol.
The diet must include:
- foods with vitamin D and calcium;
- porridge;
- boiled meat;
- light soups.
Folk remedies
Drug therapy can be supplemented with the following means:
- sea buckthorn juice;
- linden honey;
- infusion of garlic or rowan.
Important! Before starting practice, you should consult with your doctor to rule out any contraindications.
Exercises
If Cushing's syndrome is detected, you can practice light physical activity to get rid of obesity. Experts advise practicing yoga. It stimulates the immune system, restores impaired metabolism and hormonal levels.
The prognosis of Itsenko-Cushing syndrome depends on the treatment provided. If the patient refuses, irreversible changes occur, causing death in 40–50% of patients.
The outcome of the disease is determined by several factors - early diagnosis, the adequacy of the therapy, the causes of the disease, the existence/strength of complications, etc. People with Itsenko-Cushing syndrome are seen by an endocrinologist. They are contraindicated from working night shifts and heavy physical activity.
Causes
It is quite difficult to establish the exact cause of this disease, since it is extremely rare in cats.
But most doctors agree that there may be several main reasons:
- Accumulation in tissues of artificially administered cortisol, which is contained in hormonal preparations received by animals in the form of tablets or injections. If a cat is given such drugs for a long time, then disturbances in the functioning of the entire body will occur;
- Diseases of the adrenal glands resulting from tumors of the cortex and causing overproduction of glucocorticoids. As a result, the adrenal glands begin to produce excess cortisol. Almost half of these tumors are cancerous;
- Pituitary tumor. Due to its presence, a large amount of ACTH (adrenocorticotropic hormone) is formed, which stimulates the adrenal glands, which produce cortisol.
IMPORTANT! Cats should not be given medications unless necessary and without consulting a veterinarian.
Diagnostics
Only (!) in a well-equipped veterinary institution. Please note that many of the above signs can only be given by the diabetes mellitus we mentioned, and in fact, its diagnosis requires specific equipment and tools. In any case, you won’t be able to find out anything in your kitchen. Besides, Cushing is an extremely serious thing. The animal's condition quickly deteriorates without the help of specialists; not a minute can be lost!
What treatment is effective?
Drug therapy
Medicines and dosage are prescribed only by a veterinarian; self-medication is prohibited. Since Cushing's syndrome leads to brittle bones (osteoporosis), vitamin D is included in the treatment regimen, as well as medications containing fluorotridine. Doctors recommend treating hypocortisolism in cats with means such as:
The drug Mitotane may be included in the animal's treatment regimen.
- "Trilostane";
- "Metyrapone";
- "Ketoconazole";
- "Mitotane."
Surgical intervention
If hyperadrenocorticism in cats has developed due to a tumor, the following operations are performed:
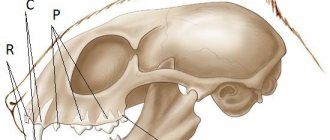
- Transsphenoidal hypophysectomy. The pituitary gland is removed by inserting an endoscope into the nasal passage.
- Adrenalectomy. The endocrine gland above the kidneys is removed. After surgery, the animal should be supported for life with hormonal drugs, which are prescribed individually by the veterinarian.
How does it manifest?
In principle, we have already described some symptoms at the very beginning of the article, but now is the time to talk about them in more detail. You should be especially wary if your pet exhibits the following:
- The cat constantly drinks and pees.
- At the same time, the animal exhibits a brutal appetite, but its weight remains the same, although its belly grows. Of course, this can also be attributed to pregnancy, but if you have a cat, it is still unlikely...
- Over time, the cat loses mobility, its muscles become weak and flabby.
- The condition of the coat is constantly deteriorating: it becomes thin and brittle, and the skin loses its elasticity. The last sign is so serious that in some animals, with the slightest mechanical impact, deep abrasions and cracks form.
Please note that the combination of all these symptoms with diabetes is a 100% guarantee of Cushing's syndrome. In the photo, such animals look very bad: severe emaciation, the skin is almost completely covered with deep, non-healing ulcers.
Adrenal insufficiency in animals - hypocortisolism
Adrenal cortex insufficiency (HYPOCORTICISM) is characterized by severe disruption of all types of metabolism due to a decrease in the synthesis of glucocorticosteroids, mineralocorticoids and androgens by the adrenal cortex.
There are primary and secondary chronic adrenal insufficiency, while primary hypocortisolism is characterized by destructive processes in the adrenal cortex, and secondary hypocortisolism is caused by a deficiency of ACTH (adrenocorticotropic hormone), which stimulates the adrenal cortex.
Causes of adrenal insufficiency
The causes of primary adrenal insufficiency include those that destroy the tissue of the adrenal cortex: fungal toxins, viral infection, tumors, autoimmune processes. Patients often have autoantibodies to adrenal tissue or to ACTH receptors. Autoantibodies to adrenal tissues are immunoglobulins of the IgM class. Primary adrenal insufficiency can manifest itself as a multimorbid disease, combined with hypoparathyroidism, thyroiditis, and diabetes mellitus. Primary adrenal insufficiency is called Addison's disease. Other causes of hypocortisolism may be amyloidosis, hemochromatosis, effects of radiation therapy, and fungal toxins.
With secondary hypocortisolism, functional insufficiency of the adrenal glands occurs due to dysregulation at the level of the hypothalamic-pituitary system (corticotropic insufficiency). In this case, a secondary decrease in adrenal activity is caused by a deficiency of ACTH produced by the anterior pituitary gland, which is dependent on corticoliberin (corticotropic releasing hormone) secreted by the hypothalamus. Secondary hypocortisolism corresponds to a deficiency in glucocorticoid production with preserved mineralocorticoid production. Primary hypocortisolism differs from secondary hypocortisolism in the dysfunction of mineralocorticoids, which is reflected in the clinical manifestation and treatment methods.
Pathogenesis. In case of the disease, insufficient synthesis of glucocorticoids is noted, and with secondary hypocorticism and mineralocorticoids, protein, carbohydrate, lipid, and mineral metabolism are disrupted. In the body, the process of gluconeogenesis is inhibited, the formation of glucose and glycogen from non-carbohydrate substances is reduced, a hypoglycemic state occurs, and poor supply of tissues with glucose occurs. With insufficient synthesis of glucocorticoids, protein synthesis in the liver is inhibited, and androgen deficiency weakens various anabolic processes. Insufficiency of ACTH secretion leads not only to atrophy of adrenal tissue, but is also accompanied by impaired secretion of gonadotropic, somatotropic, thyroid-stimulating and other pituitary hormones. Therefore, the disease takes on a polymorbid (combined) character. The excretion of sodium in the urine increases, and potassium is retained in the body. Calcium metabolism is disrupted: its absorption in the intestines increases, the release of calcium from bone tissue increases, which leads to hypercalcemia.
Symptoms. Symptoms of hypocortisolism are mild. Apathy is a common sign of the disease, anorexia, and emaciation. Hypothermia. Bradycardia does not appear constantly, but is an important sign of the disease. Muscle weakness (myopathy) and skin hyperpigmentation are noted. Against the background of general hyperpigmentation of the skin, areas of depigmentation - vitiligo - may appear, which indicates an autoimmune process. The pulse is small, soft, slow, blood pressure is low. Hypotension appears as a result of insufficient secretion of cortisol and catecholamines, depletion of the body in sodium, and a decrease in extracellular fluid (dehydration). There are signs of dysfunction of the gastrointestinal tract: nausea, vomiting, anorexia, constipation followed by diarrhea.
Laboratory tests for primary chronic adrenal insufficiency establish a sharp decrease in the blood serum sodium content and an increase in potassium (Na/K ratio below 24), a decrease in cortisol concentration, hypochloremia, hypercalcemia, uremia. The level of creatinine in the blood is increased.
Laboratory diagnosis of secondary adrenal insufficiency is very difficult and problematic in real conditions.
During pathological examination, various changes are found in the adrenal gland or in the cortex: infiltration by lymphocytes, proliferation of fibrous tissue, and in the case of an autoimmune process, atrophy of the cortical layer.
Diagnostic criteria. Muscle weakness (myopathy), decreased nutritional status. Skin hyperpigmentation. Decreased blood pressure.
Laboratory tests for primary adrenal insufficiency in the blood serum (plasma) indicate a decrease in sodium content (below 310 mg/100 ml, below 135 mmol/l), an increase in potassium above 22 mg/100 ml (above 5.6 mmol/l), creatinine above 167 µmol/l, a decrease concentrations of cortisol, aldosterone.
Treatment. The diets are filled with food rich in energy, protein, and vitamins. Table salt is added as an additive. As replacement therapy for a long time (almost for life), synthetic hormonal drugs are prescribed - cortisone acetate, prednisolone, Cortineff, hydrocortisone acetate, etc.
Cortisone acetate (adreson, cortelan) is a drug of the adrenal cortex that has a multifaceted effect. Prescribed orally for Addison's disease, acute adrenal insufficiency in therapeutic daily doses: horses, cattle 0.1-0.2 mg/kg, pigs, sheep, goats 0.3-0.5 mg/kg, dogs 0.5- 1.0 mg/kg. The daily dose is given in 2 doses. Available in tablets of 0.025 g.
Hydrocortisone acetate is a drug for the adrenal cortex. Prescribed orally in approximate doses of 0.5 mg/kg per day. Give the substance in fractions 3 times a day. The dose is selected individually.
Cortineff (fluorohydrocortisone acetate, fludrocotisone, florinef, fludrocortisone acetate) has a strong anti-inflammatory (7 times stronger than hydrocortisone) and mineralotropic effect. Used orally for primary adrenal insufficiency (Addison's disease), secondary adrenal insufficiency, and for damage to the pituitary gland - in combination with cortisone.
Prednisolone (dacortin, metacortalone, nisolone, prenalone) is a glucocorticosteroid with anti-inflammatory, desensitizing, antiallergic effects. Produced in tablets of 0.005 g, in the form of 0.5% ointment, in ampoules. Prescribed orally in approximate initial doses: dogs 0.5 mg/kg, horses, cattle 0.025-0.05 mg/kg, pigs, sheep, goats 0.1-0.2 mg/kg per day.
According to foreign data, fluorocortisone acetate and deoxycorticosterone acetate (Cortexone) are used to treat hypocortisolism in dogs and cats. Fluorocortisone acetate is prescribed orally at the rate of 10-20 mcg/kg for dogs, for cats 100 mcg per day per head. If the use of fluorocortisone acetate is ineffective, it is replaced with deoxycorona acetate, which is prescribed intramuscularly at the rate of 0.1-0.2 mg/kg once a day. Then the administration of the drug is limited to 2-3 injections per week.
Prevention. Animal owners must protect them from stress, avoid hypothermia and overheating, use of poor quality feed, underfeeding and overfeeding. Glucocorticoids are used almost for life: doses are temporarily increased in case of unfavorable factors of feeding and maintenance.
Why does pathology develop?
Cushing's disease in cats occurs due to a hormonal disorder in which the production of cortisol increases, which increases blood sugar. Cortisol is produced by the adrenal glands using adrenocorticotropic hormone. The biologically active substance also affects protein, fat and carbohydrate metabolism in the cat’s body. One of the causes of the disease is considered to be paraneoplastic syndrome, in which the adrenal gland is affected by a malignant tumor. Elevated hormone levels provoke the following factors:
- uncontrolled use of hormonal drugs by the owner;
- tumor of the pituitary gland and adrenal glands;
- age-related changes;
- frequent animal stress;
- pet poisoning with heavy metals.
Diagnosis of hyperadrenocorticism in cats
In some cases, diagnosis is made in absentia based on a history of long-term corticosteroid use, physical examination, and clinical signs.
Diagnostic testing may include routine tests such as:
- General blood analysis. It may show an increased white blood cell count.
- Biochemical profile. May reveal low calcium, elevated cholesterol, elevated glucose, elevated alkaline phosphatase and liver enzymes.
- Analysis of urine. There are three main tests that must be performed to make a definitive diagnosis of hyperadenocorticism.
- ACHT test. Its principle is based on measuring the concentration of cortisol in the cat's blood serum before and after the administration of a synthetic analogue of ACHT, which stimulates the adrenal glands.
- LDDST test (small dexamethasone test). This test is known as the ACHT suppression test. It measures the adrenal gland's response to ACHT. Dexamethasone is a synthetic steroid (cortisol analogue) that suppresses ACTH. Dexamethasone is administered and the level of cortisol in the blood is measured. Cortisol levels should decrease in response to dexamethasone. This test can help distinguish adrenal disease-based hyperadenocorticism (ADH) from pituitary hyperadenocorticism – PDH (pituitary disease).
- Urine test Cortisol:creatinine (UC:Cr). Cortisol levels are measured relative to creatine levels. If the ratio of these components is normal, then hyperadenocortisism syndrome is excluded.
- X-ray studies. These studies are useful in all cases because they allow a realistic assessment of the condition of all internal organs of a sick animal, their size, tumors, and metastases.
- Ultrasound. This may allow the veterinarian to measure the adrenal glands. In the case of spontaneous hyperadrenocorticism, the veterinarian will need to determine which of the two glands is causing the disease.