Cholangiohepatitis in cats
Cholangiohepatitis
is an inflammation of the liver and bile ducts.
The wide prevalence of cholangiohepatitis in cats is associated with the peculiarities of their anatomy: the pancreatic duct and the gallbladder ducts connect before emptying into the duodenum. Therefore, inflammation of the small intestine or pancreatitis
(inflammation of the pancreas) also leads to inflammation of the bile ducts (
cholangitis
).
Cholangiohepatitis can manifest itself in acute and chronic forms.
Acute form
occurs more often in young cats.
It begins with a sudden refusal to feed and lethargy. Vomiting appears, body temperature often rises, and the abdominal area is painful. With acute hepatitis, dehydration quickly occurs. After this, the so-called “jaundice” or icterus
(yellowish tint of the skin and mucous membranes), which is noticeable on the sclera of the eyes and gums. During this period, the activity of liver enzymes, bilirubin and the number of leukocytes in the animal’s blood increases.
Chronic form
Cholangiohepatitis is more common than acute, and older cats are more prone to it. Symptoms with this course appear and disappear in periods, with periods of exacerbation often associated with stress.
Depending on the type of cells that are found during microscopy of liver samples, chronic cholangiohepatitis may have different names. If lymphocytes predominate, it is called lymphocytic cholangiohepatitis
;
if neutrophils - then neutrophilic
;
if other defense cells (macrophages, plasmacytes) – then granulomatous
.
All forms of cholangiohepatitis can ultimately lead to liver atrophy ( cirrhosis)
).
The causes of acute cholangiohepatitis are often bacterial infections that pass to the liver from the small intestine (duodenum) and pancreas. In addition, acute cholangiohepatitis can be caused by coronavirus infection, intoxication, or feeding with low-quality or unbalanced feed.
Among the causes of chronic cholangiohepatitis, genetic predisposition comes first; it can also be due to an autoimmune disease, helminthiasis, cystoisosporosis, or malnutrition.
- Hepatic lipidosis
. Cats do not tolerate periods of not eating well (anorexia). At this time, their liver often begins to store fat, which leads to lipidosis; the functional liver tissue is irreversibly replaced by fatty tissue. Cats with a lack of appetite due to cholangiohepatitis are at risk. - Hepatic encephalopathy
. Due to increased levels of ammonia and other unwanted components in the blood, brain damage occurs. - Portal hypertension
and the formation of free fluid in the abdominal cavity (ascites). - Sometimes chronic cholangiohepatitis progresses to cancer. In humans, there has been a proven connection between chronic stimulation of lymphocytes and the occurrence of malignant lymphoma. Therefore, it is likely that chronic lymphocytic cholangiohepatitis in cats can provoke lymphoma and malignant abnormalities of lymphocytes.
- General clinical examination of the animal.
- General clinical and biochemical blood test. The presence of hepatitis or chronic inflammation of the intestines and pancreas is indicated by a high level of GGT, an increase in ALT and alkaline phosphatase with normal levels of thyroid hormones. The level of bilirubin and globulins also increases, cobalamin and folic acid decrease.
- Serological studies. Used for suspected viral infections (feline leukemia, feline immunodeficiency, feline viral peritonitis), as well as toxoplasmosis.
- X-ray examination.
- Ultrasound of the abdominal cavity (is important in diagnosing cholangiohepatitis or obstruction (blockage) of the bile duct).
- Liver biopsy. A needle is inserted through the abdominal wall into the animal's liver and material is collected for further research. The best way to diagnose hepatitis is by examining small pieces of the animal's liver. They are obtained by exploratory laparotomy (surgically) or by biopsy. Both procedures pose a certain risk and must be carried out with extreme caution, because in severe cases of the disease, the affected organs may bleed during puncture, and anesthesia poses a risk to the sick animal.
- Bacterial culture of liver and bile. If liver and bile samples can be obtained for pathological examination, it may be possible to test them for the presence of bacteria.
- stabilization of the body's condition in critical cases (intravenous therapy with electrolyte solutions). If necessary, artificial or parenteral nutrition and antiemetics are prescribed;
- antibiotics;
- choleretics and hydrocholeretics (substances that help the passage of bile from the liver to the intestines). They are prescribed to prevent bile stagnation, because this is one of the main phenomena of cholangiohepatitis;
- anti-inflammatory drugs;
- immunosuppressants (prescribed for lymphocytic portal hepatitis);
- vitamins K, E, B12. With cholangiohepatitis, the ability to absorb these vitamins through the intestines is reduced. In some cases, the use of taurine, folic acid and L-carnitine is also indicated.
The cat should be switched to a diet containing a reduced amount of sodium, carbohydrates and an increased amount of protein. It is not advisable to feed your animal food containing sucrose or fructose.
To avoid hepatic encephalopathy, if the level of ammonia in the blood of a particular animal is elevated, the amount of protein in its diet should be limited, because Protein is the main source of ammonia in the body. It is very important to feed your cat small meals multiple times throughout the day.
Neutrophilic (Bacterial) Cholangitis
Neutrophilic (bacterial) cholangitis is characterized by the infiltration of large numbers of neutrophils into the hilum of the liver and bile ducts, and is usually associated with an ascending bacterial infection, although protozoa are sometimes the cause. The causative agents of feline cholangitis include E. coli, bacteroides, actinomycetes, clostridia and alpha-hemolytic streptococcus.
Their histological distinction is based on the presence of a large number of plasma cells, lymphocytes, and sometimes macrophages in the chronic stage.
Definition of disease, spread
Among the many vital roles performed by the liver is its contribution to the digestion of food that a cat typically consumes. This digestive process relies heavily on the liver's efficient production and secretion of bile, a powerful, greenish-brown fluid that moves from the liver through the biliary system (a complex network of small channels called bile ducts) into the gallbladder. The bile is then stored in the gallbladder—a small spherical sac—until it is called to work in the intestinal tract. In response to hormonal signals, the gallbladder contracts and expels bile through the common bile duct into the small intestine, where it performs essential digestive processes such as emulsifying dietary fats so they can be absorbed from the cat's intestines and processing harmful toxins so they are expelled from the body through defecation.
Causes and mechanisms of development of feline cholangiohepatitis
Among the most common causes of liver disease is feline cholangiohepatitis
, a condition noted as inflammation of the liver and biliary system. This condition and hepatic lipidosis together account for perhaps two-thirds of all feline liver diseases presented for treatment in a typical veterinary practice.
Inflammation can have two sources, says Richard Goldstein, an associate professor of small animal medicine at Cornell University College of Veterinary Medicine. “One reason,” he points out, “is a bacterial infection that probably starts in the cat's small intestinal area—such as the pancreas or duodenum—and then in the bile tract. This problem typically causes inflammation with the migration of neutrophil blood cells, which the body mobilizes to fight bacteria. This form of infection, called feline suppurative cholangiohepatitis, responds well to antibiotic therapy, says Dr. Goldstein.
Another condition that is more common is an immune-mediated disorder that affects cells called lymphocytes. According to Dr. Goldstein, these cases (refractory to standard therapy) do not respond to antibiotics. “So we will typically treat this type of cholangiohepatitis with immunosuppressants such as steroid hormones.”
Good to know
- Microscopic studies of bacterial culture of bile samples from dogs and cats
- Histopathological overview of canine and feline liver diseases
- Clostridium perfringens and Clostridium difficile in dogs and cats
- Giardia duodenalis and Cryptosporidium spp. humans from domestic dogs
- Platynosomum fastosum infection in outdoor cats
- Histopathological changes in small animal hepatobiliary diseases
- Clinical characteristics of hepatocellular carcinoma
- Complex cholangitis/chonlangiohepatitis in cats against the background of Platynosomum fastosum infestation
- Histopathological features, immunophenotyping, cloning and eubacterial fluorescence in situ hybridization in cats with lymphocytic cholangitis/cholangiohepatitis
- Differentiating benign and malignant causes of lymphocytosis in the bone marrow
- Prognostic markers of hepatic lipidosis in cats: a retrospective study of cats
- Pancreatitis and diabetes mellitus in cats
- Feline pancreatitis and triaditis
Diagnostics
In either case, inflammation and accompanying tissue swelling interfere with the proper flow of bile, resulting in bile retention in the liver and bile ducts. And since bile is a specific digestive fluid, it can cause significant tissue damage in cases where its normal outflow from the liver is obstructed. Typical signs of cholangiohepatitis in cats include loss of appetite, fever, vomiting, and jaundice (which can cause the sclera of the eyes to become icteric).
Because these clinical signs of feline cholangiohepatitis
Similar to those associated with other serious liver diseases such as liver cancer, feline infectious peritonitis, and hepatic lipidosis, a variety of complex diagnostic tests may be required to reach a definitive diagnosis of cholangiohepatitis. In addition to a complete blood count, blood chemistry panel, and urinalysis, these tests may include abdominal x-rays and ultrasounds; bile acid analysis; and a test to determine blood clotting ability. In some cases, an exploratory laparotomy will be necessary to examine the liver and gallbladder. If a preliminary diagnosis of feline cholangiohepatitis is made, a liver biopsy may be performed to confirm the diagnosis. A liver biopsy will also differentiate between types of cholangiohepatitis, an important point since treatment varies depending on the type of cholangiohepatitis diagnosed.
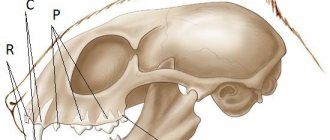
Definition, terminology
Cholangitis in cats
- inflammation concentrated in the biliary tree (bile ducts), a common form of liver disease, and apparently the second most common after lipidosis. A new simplified classification scheme proposed by the WSAVA Liver Diseases and Pathologies Standards Study Group suggests 3 different forms of cholangitis in cats:
- Neutrophilic (Bacterial) Cholangitis
- Lymphocytic Cholangitis
- Chronic Cholangitis
The new proposed classification scheme also prefers the term "cholangitis" to "cholangiohepatitis" since inflammatory parenchymal lesions are not always present and, if present, are a complication of primary cholangitis.
Prognosis of cholangiohepatitis in cats
In general, the prognosis of cholangiohepatitis in cats is unpredictable. If diagnosed early in the disease, some cats with the suppurative form of the disorder may respond well to antibiotic therapy and eventually return to normal. And long-term remission is possible in cats that are effectively treated for the refractory type. However, the prognosis is poor for cats diagnosed with any type of cholangiohepatitis when it has already reached a more advanced stage. Severe cholangiohepatitis can progress to biliary cirrhosis, in which vital bile duct tissue is replaced by tough connective tissue. Although biliary cirrhosis is considered the final stage of severe cholangiohepatitis, it is rarely seen because cats with severe disease and those misdiagnosed rarely live long enough to develop it. Prompt diagnosis and treatment will increase the likelihood that treatment will be successful.
Clinical signs of cholangitis in cats
https://www.youtube.com/watch?v=ytcopyrightru
Clinical signs of cholangitis in cats associated with inflammatory liver disease are variable and nonspecific, and are sometimes the same as those seen in hepatic lipidosis. Partial or complete anorexia is more common, and sometimes this is the only symptom. Other less common symptoms include weight loss, lethargy, vomiting, diarrhea and fever.
Cats that develop acute cholangitis are younger (mean age 3 years) than cats with chronic cholangitis (mean age 9 years) or hepatic lipidosis (mean age 6.2 years). Males are more susceptible to acute neutrophilic cholangitis. Cats with acute cholangitis are more severely ill than cats with other liver diseases.
The signs of the disease in their clinical manifestations are similar to pathologies of the liver structures. It is possible to develop non-specific symptoms, which complicates the initial diagnosis.
The most common symptom of neutrophilic or lymphocytic cholangitis in cats is refusal to eat food and the inability to digest it normally (anorexia). Less common are signs such as rapid weight loss, eruption of gastric contents, fever and profuse diarrhea.
The occurrence of characteristic symptoms of cholangitis - eruption of gastric contents, apathetic state, yellowness of visible mucous membranes - requires immediate contact with a specialist. In a veterinary clinic, after ordering laboratory tests, the doctor prescribes treatment. First of all, the doctor conducts a clinical examination, collects anamnesis and prescribes tests.
The following studies are prescribed:
- blood biochemistry and general clinical blood test;
- urine analysis;
- X-ray of organs located in the abdominal cavity;
- ultrasound diagnostics;
- biopsy of liver cellular structures;
- diagnostic laparoscopy.
With cholangitis, a blood test will indicate increased bilirubin, low iron-containing protein, high bile acids and white blood cells. An ultrasound examination reveals a pronounced change in the size of the liver, obstruction of the biliary tree and stagnation of bile acids. Laparoscopic examination can detect changes in the liver, as well as visualize the gallbladder.
Feline cholangitis syndrome
Feline cholangitis syndrome
Cholangitis is an inflammation of the bile ducts, manifested by indigestion and jaundice.
The main cause of inflammation of the biliary tract is microflora that penetrates from the duodenum through the bile duct, portal vein and hepatic artery. Often the disease occurs as a complication of infectious (colibacillosis, salmonellosis) and parasitic (fascioliasis, dicroceliosis, eimeriosis) diseases. Inadequate diets, especially in vitamin A, as well as feed toxicoses contribute to the development of the disease.
Cholangitis in cats is relatively common and is very different from liver disease in dogs. It can be quite difficult to treat, especially if the cause of the disease is not precisely known.
There are three main types of cholangitis in cats:
Neutrophilic cholangitis is caused by a bacterial infection in the liver, leading to inflammation. Usually develops as a result of migration of bacteria to the bile ducts from the small intestine. The disease is sometimes observed simultaneously with inflammation of the pancreas and intestines.
Lymphocytic cholangitis is non-infectious in nature, although it also leads to inflammation. The exact cause is unknown, but the disease may be related to disturbances in the cat's immune system (immune-mediated disease).
Lymphocytic cholangitis presents with typical chronic tissue changes progressing over months or years and may initially be asymptomatic. The disease is more common in younger and Persian cats. The pathophysiological mechanisms of its development are unknown, but they are assumed to be immune-mediated.
In the third case, the disease develops against the background of opisthorchiasis, a parasitic disease.
Endocrine glands
Clinically, the disease can manifest itself as drowsiness, loss of appetite, vomiting, weight loss, and bloating due to effusion into the abdominal cavity. On palpation and percussion there is severe pain in the liver area. In most cases, signs of obstructive jaundice appear due to obstruction in the outflow of bile. However, sometimes the cat’s condition does not correspond to the diagnosis at all, and the appetite even increases.
Characteristic diagnostic signs of cholangitis are increased levels of alkaline phosphatase; hyperbilirubinemia; increased levels of bile acids in the blood serum. In some cases, neutrophilia with a shift to the left is possible.
Ultrasound examination can reveal thickening of the gallbladder wall and bile stagnation. However, sometimes the ultrasound picture is completely normal. In some cases, the liver tissue is hyperechoic. If bile stagnation occurs, the echogenicity or size of the common bile duct may increase.
Differential diagnosis
Ultrasound of the gallbladder
- Liver lipidosis,
- Acute toxic hepatopathy,
- Feline infectious peritonitis,
- Hyperthyroidism,
- Toxoplasmosis,
- Bartonellosis,
- Portosystemic shunting,
- Extrahepatic biliary obstruction,
- Neoplasms (bile duct cancer, hepatocellular carcinoma, lymphoma), tumor metastases.
The basis for the treatment of cholangitis in cats is properly selected antibacterial therapy. Since infectious agents most often come from the gastrointestinal tract, the optimal choice would be a powerful broad-spectrum antibiotic that is bactericidal and active against anaerobes. It is desirable that this antibiotic is excreted primarily in bile.
Traditionally, treatment begins with the prescription of corticosteroids , both to suppress inflammation and, thereby, immune-mediated liver damage, and to protect against the development of fibrosis.
In addition to primary treatment for cholangitis in cats, supportive or additional treatments may be effective:
- Intravenous hydration and electrolyte administration
Fluids and electrolytes should be selected according to the electrolyte profile. Crystalloids should be given initially for rehydration and maintenance. If the cat's liver dysfunction is more severe, or cirrhosis has developed, hypoproteinemia may be present. In these cases (usually accompanied by ascites), treatment with colloids is recommended.
The liver produces blood clotting factors; when its function is impaired, there is a risk of developing coagulopathy (blood clotting disorder). With cholestasis (stagnation of bile), the absorption of vitamin K in the intestine is impaired, which further aggravates the blood clotting disorder.
Treatment
Therapy for cholangitis in cats involves the use of medications. If the bile ducts are obstructed, surgery is performed. Emergency surgery is performed if signs of peritonitis appear.
Among medications, antibiotics are of primary importance. They are prescribed for the treatment of any type of cholangitis. In therapy, amoxicillin (for the activity of anaerobic bacteria) and aminoglycosides (for the activity of anaerobic infection) are most often used. Contraindication is the use of tetracycline, which has hepatotoxic properties.
In the treatment of lymphocytic and lymphoplasmacytic type, immunomodulators (prednisolone) are used.
Vitamin K is prescribed in case of increased blood clotting time.
To maintain liver function, it is possible to use hepatoprotectors. They prevent the destruction of cell structures and stimulate their regeneration.
During the treatment process, it is necessary to improve the cat's nutrition. It is recommended to use easily digestible food (or natural food) with a low protein content.
Cholangiohepatitis in a cat
When the bile ducts and liver become inflamed, cholangiohepatitis occurs in cats. The disease has an acute and chronic course and is accompanied by vomiting, jaundice of the mucous membranes, and hyperthermia. If the pet's health deteriorates, the owner is obliged to show it to a veterinarian, who will conduct a diagnosis, prescribe medications and nutritional therapy, which determines the prognosis.
Based on their practice, veterinarians are confident that cholangiohepatitis can provoke irreversible processes in the liver, such as cirrhosis.
Etiology and pathogenesis: what are the causes of the disease?
The main factor in the appearance of cholangiohepatitis in cats is cholangitis - inflammation of the bile ducts. This is facilitated by the entry of coliform bacteria or staphylococcus from the intestines into the liver ducts to remove bile. In advanced cases, microbes spread to the digestive gland. Often the pathology is provoked by triaditis - simultaneous inflammation of the intestines (enteritis), bile ducts (cholangitis) and pancreas (pancreatitis). The pathogenesis of cholangiohepatitis also includes infection with helminths - opisthorchiasis. The bile ducts are blocked by parasites, which disrupts the production and flow of bile and causes cholestasis. Main reasons:
Symptoms of cholangitis and cholangiohepatitis in cats
The cholangitis/cholangiohepatitis complex is a series of associated inflammatory or infectious diseases of the liver as well as the biliary tract.
Cholangitis refers to infection or inflammation of the bile duct, and cholangiohepatitis is inflammation of the biliary system and, in particular, the liver parenchyma around the bile ducts. The clinical signs of these diseases in this complex are similar and include:
- Jaundice (yellowing of the skin, sclera of the eye and mucous membranes)
- Lethargy
- Anorexia
- Vomit
- Fever is common in acute form but rare in chronic form.
- Dehydration
- Diarrhea
- Ascites (fluid in the abdominal cavity) sometimes occurs due to cirrhosis
Symptoms: how to recognize the disease?
During the inflammatory process, the liver structures are attacked by cells, so the disease is divided into granulomatous, neutrophilic and lymphocytic. Veterinarians distinguish 2 forms of cholangiohepatitis in cats:
- Acute, in which the disease begins suddenly and is acute.
- Chronic, characterized by a period of remission and exacerbation.
Depending on the type of disease, the symptoms differ as shown in the table:
| Pharmgroup | Veterinary medicine |
| Hepatoprotectors | "Hepatovet" |
| "Divopride" | |
| "Vet Expert" | |
| "Gepasafe" | |
| Antibiotics | "Marfloxin" |
| "Amoxicillin" | |
| "Sinulox" | |
| Antiemetics | "Cerucal" |
| Choleretic | "Allohol" |
| Vitamins | Injections of vitamin E, K, B12 |
Return to contents
Medical nutrition
If the liver and bile ducts are inflamed, treats from the table, fried, smoked, and salted should be excluded from the cat’s diet. It is recommended to switch the animal to dietary food:
- Royal Canin Hepatic;
- Hills Diet Felin;
- "Farmina Hepatic";
- "Purina Pro Plan Veterinary Diets Hepatic."
At the same time, you can give the animal the following products:
- lean meats and fish that have undergone heat treatment;
- lean broth;
- carrots or potatoes, steamed or boiled;
- rice or oatmeal porridge with water;
- low-fat dairy products.
Return to contents
Treatment at home
Therapy with herbal remedies can only be carried out after consultation with a veterinarian, but it should not replace traditional treatment.
To restore the functions of the liver and bile ducts, chamomile, yarrow, dandelion root, nettle, and plantain are used. You can use ready-made feed mixture “Fitomina”. A decoction of herbs that should be gradually infused into the cat using a syringe without a needle is effective. Preparation:
- Take 5 g of any plant and pour 200 ml of hot water.
- Let it brew for 20-30 minutes, cool, filter.
- Dilute the resulting broth with cool water.
- Give the cat 5 ml 3 times. in a day.
Return to contents
Prognosis and prevention
Timely detection and treatment of cholangitis gives a chance for a favorable prognosis. However, the chronic form can cause cirrhosis. In advanced cases, the purulent type of the disease leads to the death of the animal. Undiagnosed opisthorchiasis is also dangerous, when helminths can settle not only in the bile ducts, but also in vital organs, which provokes death.
To avoid cholangitis in a cat, it is recommended not to give your pet meat and fish that have not undergone heat treatment, and to regularly deworm it. The weight of the animal should be monitored and the correct diet should be ensured. This will help prevent the formation of stones. All pathologies that can cause the disease must be treated in a timely manner.