Hyperparathyroidism in cats is a disease associated with a metabolic disorder (metabolic process), when calcium is washed out of bone tissue and enters the bloodstream. In accordance with the physiological norm, 99% of its volume is contained in the structures of the skeleton and tooth enamel, and the remaining 1% is present in the form of ions in the blood. With hyperparathyroidism, the balance is disrupted, which causes pathological changes in the body. Read more about the symptoms and treatment of this disease in our article.
Hyperparathyroidism in cats: symptoms and treatment
What is hyperparathyroidism in cats: symptoms
The disease hyperparathyroidism in cats is characterized by brittle bones due to metabolic disorders. This also happens due to an excess of calcium in the body and a lack of phosphorus, which, in turn, provoke the development of bone dystrophy.
Reference!
During the course of the disease, bone tissue is “resorbed”, and calcium from the bones moves into the blood and is simply excreted from the animal’s body in the urine.
Thus, the animal’s bones are simply not able to withstand any loads. But that's not all! As the kidneys process large amounts of calcium, he develops urinary stones, which further aggravates the situation.
The initial stage of the disease is not characterized by the presence of any pronounced symptoms. That is, you most likely won’t notice anything right away. However, if you discover weakness, depression and not the best mood in your pet, then it is better to keep your ears open.
If, after all, the animal has this particular disease, then everything will become clear from the following symptoms:
- constant thirst (the animal will drink a lot);
- frequent urination (you can read about how to teach a cat to go where it’s supposed to go here);
- decreased appetite (which can also be a sign of eye disease).
In later stages appear:
- lameness;
- paralysis of limbs;
- curvature of limbs;
- swelling and pain of joints;
- loosening and loss of teeth;
- bone fractures.
Important!
To determine the presence of the disease, the animal must undergo a blood test to determine the content of calcium and phosphorus in it and conduct an X-ray examination.
There are several types of disease. Next, we will get acquainted with the types of hyperparathyroidism and tell you how to cope with it.
Symptoms in puppies and kittens, adults
This insidious disease has uncharacteristic clinical signs and is often mistaken for rickets in young animals. The owner should carefully monitor the health status and know the symptoms of hyperparathyroidism in dogs:
- Growth retardation compared to breed standards.
- The activity of the young pet is reduced. The puppy does not want to take part in games. The owner often experiences drowsiness and lethargy.
- Curvature of the bones of the limbs and spine.
- Permanent fractures.
- The deposition of calcium salts in the synovial membranes leads to severe pain.
- After jumping, active movement, or running, the dog experiences lameness.
- Chronic constipation.
Weakness of the hind legs
With hyperparathyroidism in cats, the owner may observe the following symptoms:
- Loss of activity.
- Decreased appetite.
- Nausea, bloating.
- Loss of teeth.
- Pain when stroking.
- Skeletal deformation.
- Numerous fractures.
- Neurological manifestations: paresis, convulsions.
Against the background of metabolic disorders in the body, cats often develop urolithiasis and heart problems.
Symptoms
Eclampsia in a cat has very specific symptoms, but sometimes they can be confused with signs of nervous disorders. That is why you cannot prescribe treatment to an animal yourself; this should be done by a specialist after conducting a series of tests and analyses. Particularly important is a blood test that will show the concentration of calcium in the blood.
After giving birth, it is necessary to monitor the animal very carefully in order to see in time that she is developing eclampsia. In cats, symptoms of this disease may include the following:
- the pet behaves inappropriately, she looks as if lost;
- mastitis appeared;
— the cat’s mood changes sharply from horror to happiness;
- decreased temperature;
- coordination is impaired;
- dilated pupils;
- convulsions.
Just yesterday, a friendly cat can today begin to hide from everything and everyone, including her own kittens. Immediately she can rush to the offspring, dragging the cubs one after another, transferring them to other places. Eclampsia in a cat can also manifest itself in the fact that it begins to bite itself, bite kittens, and be in fear all the time. Sometimes this behavior even ends with her eating her offspring.
Approximately 8-12 hours after the first signs of the disease appear, the muscles lose their elasticity and become stiff. For this reason, the cat can take strange poses, bend, trying to eliminate this inconvenience.
Treatment of the disease
The scheme of therapeutic intervention is largely determined by the stage to which the pathology has progressed. Veterinarians distinguish primary and secondary nutritional hyperparathyroidism, each of which has its own specific characteristics and requires a specific type of treatment.
Primary form
It is important to understand that when the first signs of the disease appear and its subsequent diagnosis, the cat will need a carefully prepared diet, including ready-made food. This measure is justified by the fact that they are created under the supervision of specialists, which means they contain all the microelements and vitamins a cat needs. In some cases, the pet is prescribed a diet made up exclusively of natural products. It should be noted right away that the owner should not try to compile it on his own; it is better to use the help of the attending physician.
This form of the disease is quite easy to get rid of through surgery. Its essence is for the veterinarian to remove the damaged lobes from the animal, and also to minimize the production of parathyroid hormone, thereby reducing the release of calcium into the blood and preventing the microelement from being sucked out of the bones. Owners should be prepared for the fact that the cat will spend the next week after the operation under the supervision of a doctor. He will monitor your pet's calcium levels in the bloodstream daily.
Secondary hyperparathyroidism
It is divided into kidney and food varieties. Treatment for each of them is strictly individual and depends on many factors, such as weight, age and general condition of the pet. The beginning of therapy consists of restricting the cat's movement. To do this, it is placed in a special container for a period of no less than 3-4 weeks. In addition, a diet is developed that includes all the vitamins and minerals the patient needs.
The food variety is treated with pharmaceuticals. Such means for improving the condition of bones as Travmatin and Chondartron have proven themselves well. Additionally, the cat is prescribed courses of vitamins that promote the absorption of beneficial components from the food it absorbs. The disease is aggravated by chronic constipation, so the animal will need to take Vaseline oil to soften the stool.
The renal subtype of the disease is treated with the same methods, only with one condition - you need to reduce the level of phosphorus in the circulatory system and reduce its absorption from the gastrointestinal tract. Owners must understand that such a dangerous disease cannot be cured in two days, so they must be patient and carefully follow all the specialist’s recommendations.
Diseases of the endocrine system can negatively affect the quality of life of a mustachioed pet. You can protect yourself from them with the help of a properly composed menu for your pet and regular examinations by a veterinarian. At the first signs of hyperparathyroidism, you should take your pet for examination to a specialist. Ignoring the problem can lead to disability and death for the cat.
Primary: diagnosis
The primary disease appears as a result of certain diseases, namely:
- cancer;
- adenomas;
- glandular hyperplasia.
Diagnosis and symptoms
The disease is diagnosed in the clinic, a blood test is performed and, if necessary, an x-ray is taken.
Symptoms in the early stages are mild. Typically, the animal is lethargic, eats little and does not move much. For some animals this behavior is the norm, while for others it is the opposite. Knowing his pet, the owner will certainly be able to determine whether everything is normal with him.
Peculiarities
In the mildest cases, the peculiarity is that treatment as such is not required. It is enough to switch to proper nutrition, preferably premium. Your veterinarian will tell you which food to choose in this particular case.
Treatment
The primary stage is easily treatable with proper feeding.
Attention!
After just a few months of proper nutrition, the balance of phosphorus and calcium in the body is restored.
If the disease has developed, for example, due to an adenoma, then surgical intervention will be required.
Useful video
Watch this video about the causes and treatment of hyperparathyroidism in cats and dogs:
Similar articles
- The dog does not have enough calcium: reasons for the deficiency...
It is possible to identify that a dog does not have enough calcium by characteristic symptoms, including convulsions, tachycardia, tremors and others. Read more - Rickets in cats: symptoms, treatment at home...
One of the most common diseases is rickets in cats. The earlier treatment is started, the greater the chances of saving the kitten even at home. After rickets in childhood, the kitten should be monitored throughout its life. Read more
- Fracture of the jaw in a cat: x-ray of the lower...
bites from relatives or dogs; careless handling of an animal .serp-item__passage{color:#888}… hyperparathyroidism is a metabolic disease associated with a decrease in calcium in the animal’s body. The consequence of the disease is fragility of bones and their frequent… Read more
- Arthritis in cats: symptoms, treatment methods, cure...
Arthritis occurs in cats due to a number of factors. Symptoms do not appear in the initial stages, making diagnosis difficult. Treatment involves taking medications to relieve pain and restore cartilage. Read more
- Goiter in a dog: what to do if endemic...
A dog may develop a goiter due to a lack of iodine. It can be endemic, toxic and several other types. It looks like a growth on the neck. What to do and how... Read more
Treatment
Treatment must be started immediately. It consists in saturating the body with calcium. However, it must be remembered that its excess is just as harmful as its deficiency. Therefore, only a doctor can prescribe medications and recommend doses.
So, if you notice signs of the disease, you should immediately contact a veterinarian. Before taking, you can administer one and a half cubes of calcium gluconate and 3 cubes of Gamavit. If you notice that a cat is licking, pulling, or biting kittens, they should be separated for about a day.
In case of severe illness, the animal will be left in the clinic for several days. Eclampsia in cats, treatment of which is started early, goes away quite quickly. The animal is injected with a calcium solution intravenously. If you do injections at home, you should remember a few simple rules:
— at home, the drug is administered only intramuscularly;
— it is better to purchase “human” calcium, it is absorbed by cats much better than veterinary calcium;
- injection must be done in different places, changing limbs each time;
— calcium must be heated to a temperature higher than room temperature, so before administration, the syringe should be held in your hands for several minutes.
Treatment of hyperparathyroidism in dogs and cats
If nutritional hyperparathyroidism is detected in puppies, the first thing a veterinarian recommends is a review of the diet. The diet of a sick individual should be complete, with a high content of calcium in foods. The level of phosphorus in the diet is minimized. When feeding natural food, the animal is given different types of meat: chicken, beef, rabbit.
The puppy should receive fermented milk products at least once a day. Low-fat cottage cheese, fermented baked milk, yogurt, cream and natural yogurt can serve as a source of calcium.
Along with calcium, the body of a young animal should receive a sufficient amount of vitamin D. The pet should be given regular sunbathing. On the recommendation of a veterinarian, vitamin supplements are introduced into the puppy’s diet: meat and bone and fish meal, vitamin D concentrate, fish oil.
If primary hyperparathyroidism is detected in an animal, then surgical removal of the tumor may be considered. Surgical intervention is reduced to resection of the damaged lobes of the parathyroid gland and is carried out in specialized institutions.
When hyperparathyroidism is detected in kittens, their activity is first limited. To do this, the sick pet is placed in a small box, cage or crate. This is done to prevent spontaneous fractures. For the entire treatment period, which can be 2-3 months or more, the animal is prescribed therapeutic food enriched with calcium.
The best option would be to use specialized feeds that take into account the low need of the sick organism for phosphorus and the high need for calcium.
Treatment of metabolic disorders in advanced cases cannot be done without the use of medications. For example, borogluconate, calcium gluconate, calcium chloride are injected intravenously into the body of a sick pet.
Therapy for hyperparathyroidism in pets, in addition to enriching the body with calcium, also includes symptomatic treatment. Thus, sick animals often suffer from chronic constipation. Vaseline oil can help solve the problem.
We recommend reading about the causes of goiter in dogs. From the article you will learn about the types of pathology, symptoms of goiter in dogs, diagnosis and treatment.
And here is more information about the manifestations and treatment of Cushing's syndrome in dogs.
Such a serious metabolic disorder in four-legged family members as hyperparathyroidism often develops as a result of gross violation of the rules of feeding young animals. A deficiency of calcium and vitamin D in the diet and an excess of phosphorus are the main causes of the nutritional form of the disease. In cats, the disease often occurs against the background of chronic renal failure.
Treatment includes, first of all, dietary nutrition, the introduction of minerals and vitamins into the body of a sick pet. If neoplastic processes are detected, a veterinarian performs surgical removal of the damaged lobes of the parathyroid gland.
Secondary
Secondary hyperparathyroidism is called juvenile osteopathy. It occurs due to a lack of calcium. Also, it may appear after certain illnesses:
- destructive kidney damage;
- chronic dystrophic changes in the small intestine.
Important! As sad as it may be, primary hyperparathyroidism is much more common.
There are several types of this form of the disease, namely: nutritional and renal.
Nutritional
The nutritional type occurs due to improper nutrition, that is, it is provoked by the owner himself. A balanced diet specially formulated for cats will have calcium and phosphorus levels in the correct (healthy) ratio. If a person feeds the animal “from the table,” then problems arise with the content of these substances in the body and, in the future, hyperparathyroidism develops.
Important!
The disease develops rapidly due to feeding the cat meat or dairy foods.
These products contain several times more phosphorus than calcium. This provokes the development of the disease.
Diagnosis and symptoms
Diagnosing the disease is quite simple since the symptoms of the disease are very pronounced, but owners sometimes do not pay attention to their pets. Most often, hyperparathyroidism is discovered in the clinic due to some kind of injury. For example, a broken limb, and the animal does not have to fall from a great height. At this stage, it is enough to jump from a height of half a meter.
Attention!
To determine the disease, blood collection will be required.
Symptoms:
- hypersoreness;
- tooth loss;
- softening of the jaw (becomes soft to the touch).
Due to the fact that the pet feels pain and aching bones, he refuses to run and play. Often shows aggression while stroking. Spends a lot of time lying or sitting, while looking constantly lethargic.
Peculiarities
A feature of the disease is a genetic predisposition. Siamese and British cats are most often affected.
Treatment
Treatment involves proper, balanced nutrition with a low phosphorus content and, of course, the use of medications.
Important!
Medicines are prescribed by the doctor based on the patient’s tests!
Renal
Renal hyperparathyroidism develops in those individuals who have kidney problems. With this form, the phosphorus content in the blood increases, and calcium, on the contrary, decreases. Diagnosis and symptoms The disease can be diagnosed by symptoms:
- dehydration;
- polyuria (increased urine production);
- polydipsia (unquenchable thirst);
- weakness;
- vomit;
- loss of appetite;
- lameness in various limbs.
However, a doctor must make an accurate diagnosis and prescribe treatment. Diagnosis is carried out in the clinic. For this we use:
- visual inspection;
- X-ray.
On x-rays, bones are most often barely visible. They become depleted and become transparent. The older and heavier the pet, the more serious the consequences can be.
Peculiarities
Features of the disease are:
- constipation;
- heart problems;
- problems with cardiac activity;
- limb failure.
Treatment
Here, treatment also begins with drawing up the right diet, and further actions depend on what tests are performed. The cat will need either drug treatment and mineral supplements, or surgical intervention.
Types of pathology
In veterinary practice, it is customary to distinguish between primary and secondary diseases.
Primary and secondary (alimentary)
Primary hyperparathyroidism in dogs is caused primarily by pathological changes in the thyroid gland, which produces parathyroid hormone. According to the observation of veterinary specialists, older dogs most often suffer from the primary form of the disease. Cats get sick less often.
Oncological processes (adenoma, malignant tumors), hyperplasia of the parathyroid gland are the main causes of the development of the primary form of impaired parathyroid hormone production in domestic animals.
A secondary metabolic disorder caused by increased production of parathyroid hormone is associated with impaired renal function. Mainly cats suffer from this form of the disease due to the development of chronic renal failure. In case of kidney disease, a disturbance in the electrolytic balance occurs in the animal’s body: the concentration of calcium in the blood decreases, and the level of phosphorus increases.
As compensation, the parathyroid gland intensively produces parathyroid hormone, which has little effect on calcium levels. In addition, the content of calcitriol in the body decreases, which is accompanied by impaired mineralization of bone tissue.
Nutritional
Most often we encounter nutritional hyperparathyroidism in dogs and cats, caused by errors in feeding. The disease develops against a background of low calcium levels and increased doses of phosphorus in the animal’s diet. Young pets with a high need for building material for bones are the main risk group for nutritional hyperparathyroidism.
A lack of calcium, magnesium, vitamin D and an increased content of phosphorus in foods during the active growth of the skeleton of kittens and puppies leads to a gross disruption of mineral metabolism. The reason for this imbalance is often a mono-diet - feeding a young animal only meat, for example, chicken.
A malabsorption of calcium and vitamin D from the intestine as a result of prolonged diarrhea can also lead to the nutritional form of the disease.
Juvenile
Often, cat owners may hear from a veterinarian that their animal has juvenile hyperparathyroidism. This is the term that professionals call the secondary form of pathology in furry patients.
Secondary hyperparathyroidism and its varieties
The secondary form of the disease is not associated with dysfunction of the parathyroid gland. A completely healthy organ produces the required amount of PTH, but the very need for it, for various reasons, is formed incorrectly. This form is alimentary (food) and renal. Their similarities and differences are described in the table:
| Form of secondary hyperparathyroidism | Who is susceptible | Cause | Characteristic symptoms |
| Nutritional | Kittens | Feeding your pet meat and offal without bones and calcium-containing products | Refusal to move, injury as a result of jumping or falling from a small height (20–30 cm) |
| Renal | Animals of any age with impaired renal function | Inability of the kidneys to remove excess phosphorus and produce calcitriol, the active form of vitamin D that controls calcium metabolism | In addition to bone destruction, kidney and brain damage has been observed |
The occurrence of secondary hyperparathyroidism in kittens is facilitated by poor nutrition of a pregnant cat, early weaning of babies from their mother, and helminthic infestations. In adult animals, predisposing factors are also diseases of the digestive system, thyroid gland, as well as excess food vitamins A and D, phytin, magnesium and fluorine.
Alimentary (secondary) hyperparathyroidism (nutritional or juvenile osteodystrophy) - Vasiliev A.A.
NUTRITIONAL (SECONDARY) HYPERPARATHYROSIS (NUTRITIONAL OR JUVINYL OSTEODISTROPHY)
- an endocrine disorder characterized by excessive synthesis and secretion of the parathyroid hormone parathyroid hormone, which is involved in the regulation of extracellular calcium levels. Secondary hyperparathyroidism is a disease that occurs as a result of prolonged stimulation of the parathyroid glands by a reduced level of calcium in the blood, initially as a compensatory process, and then a chain of pathological processes occurs that develop in response to a chronic decrease in the level of calcium in the blood (hypocalcemia). The parathyroid gland controls the level of calcium in the blood, a hormonally caused disorder leads to impaired bone mineralization and improper skeletal development, which is a consequence of poor nutrition when kittens or puppies do not get enough calcium in their diet. A diet consisting mainly of meat and organ meats such as heart, liver and kidneys, etc. contains too high levels of phosphorus and very little calcium and vitamin D (vitamin D is necessary for the absorption of calcium in the small intestine), which leads to impaired growth and development of the skeleton, spontaneous fractures and lameness.
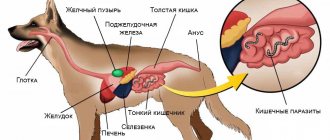
Exchange of calcium and phosphorus in the animal's body.
Calcium is one of the essential elements in the life of mammals. Calcium homeostasis is a very complex, balanced and multicomponent mechanism, the main links of which are calcium receptors on cell membranes that recognize minimal fluctuations in calcium levels and trigger cellular control mechanisms (for example, a decrease in calcium leads to an increase in the secretion of parathyroid hormone and a decrease in the secretion of calcitonin), and effector organs and tissues (bones, kidneys, intestines) that respond to calcium-tropic hormones by correspondingly changing Ca++ transport.
The main hormonal mediators of calcium homeostasis are parathyroid hormone, vitamin D and calcitonin.
Parathyroid hormone, produced by the secretory cells of the parathyroid glands, plays a central role in calcium homeostasis. Its coordinated actions on bones, kidneys and intestines lead to an increase in the transport of calcium into the extracellular fluid and an increase in the concentration of calcium in the blood.
Parathyroid hormone has both anabolic and catabolic effects on bone tissue, which can be distinguished as an early phase of action (mobilization of Ca++ from bones to quickly restore balance with extracellular fluid) and a late phase during which the synthesis of bone enzymes (such as lysosomal enzymes) that promote resorption and remodeling of bone tissue. The primary point of application of parathyroid hormone in bones is osteoblasts. Under the influence of parathyroid hormone, osteoblasts produce a variety of mediators that have a powerful stimulating effect on the differentiation and proliferation of osteoclasts. Thus, bone resorption by osteoclasts is stimulated indirectly through osteoblasts.
Vitamin D is the second strong humoral agent in the system of regulation of calcium homeostasis. Its powerful unidirectional effect causes an increase in calcium absorption in the intestines and an increase in the concentration of Ca++ in the blood.
ETIOLOGY, PATHOGENESIS OF HYPERPARATHYROIDSIS
The metabolism of calcium is closely related to the metabolism of phosphorus (mainly phosphate -P04), and their concentrations in the blood are inversely related. The ratio of calcium to phosphorus in the diet should be no less than 1:1 for dogs and 0.9:1 for cats and should not exceed 2:1 for both species. In the blood, the ratio of calcium and phosphorus for dogs and cats from 3-9 months. – 0.9-1.3, over 9 months. – 1.6-2.3.
The disease is observed in small kittens and puppies, which are fed primarily with meat or offal, because Meat food contains a lot of phosphorus and little calcium, which leads to a violation of the mineralization of the skeleton, its deformation, and in the case of a long course of the disease, fractures of the limbs. A calcium-poor diet stimulates the production of parathyroid hormone, as a result of which the deposition of calcium salts in the bones decreases, and the body begins, on the contrary, to take calcium from the bones (osteoresorption) in order to maintain a normal level of calcium in the blood.
In turn, insufficient calcium intake is often reported when feeding dogs and cats diets consisting of meat or meat by-products. Typically, meat diets contain approximately 0.02% Ca and 0.3% P, which provides a Ca to P ratio of 1:15–1:20, which causes secondary hyperparathyroidism.
The maximum osteoresorptive effect is observed in bones with a pronounced cortical structure (long tubular bones), while bones with a trabecular structure (vertebrae, iliac crest) can maintain their density. This effect has a certain differential diagnostic significance when, during an X-ray examination of patients with secondary hyperparathyroidism, a decrease in bone density is recorded in the area of the radius and tibia, less in the femur and often absent in the vertebrae.
Vivid clinical manifestations of bones are accompanied by cases of secondary hyperparathyroidism in young, actively growing animals. In them, the effect of excess parathyroid hormone manifests itself faster - deformations of the bones of the limbs, spine, fractures, etc. occur. A clear example is the clinical case of the cat Ushlepa, who was admitted to the clinic for observation by orthopedic doctors regarding X-shaped curvature of the lower extremities, thoracic lordosis, lumbar kyphosis and pelvic canal stenosis, the cause of which turned out to be severe primary hyperparathyroidism caused by a mono-diet (feeding meat birds).
Joints are also a weak link in the body of patients with primary hyperparathyroidism. The load on them increases due to erosive changes in the epiphyses and disruption of bone geometry. Another pathogenetic factor of arthropathy is the deposition of calcium salts in the synovial membranes, cartilage and periarticular, which leads to chronic trauma and severe pain throughout the life of the animal.
Neuromuscular changes in secondary hyperparathyroidism manifest themselves in weakness and fatigue. This is a reversible syndrome that quickly disappears after adequate help is prescribed.
CLINICAL SIGNS
The disease has a long-term hidden nature of development, the absence of pathognomonic symptoms up to the development of severe osteodystrophy with destruction of the skeleton. As a rule, the disease manifests itself between the ages of 3 and 7-8 months; purebred cats (Scottish, British, Sphynx, exotic) are often affected.
• Reduced activity and mobility, lack of interest in games, drowsiness;
• Lameness, even after jumping or falling from a small height;
• Incorrect positioning of the limbs (X-shaped);
• Constipation;
• Neatness of movement, lack of playfulness, curiosity and desire to “walk on the ceiling” characteristic of cats; the animal has difficulty overcoming obstacles and jumping on furniture.
Lameness is the most indicative symptom of the disease. The cause of lameness is calcium deficiency in the bones, as a result of which their fragility increases and stress tolerance decreases. In extremely severe conditions, subperiosteal greenstick fractures are possible.
LABORATORY DIAGNOSTICS OF SECONDARY HYPERPARATHYROIDIS
The key criteria for the laboratory diagnosis of hyperparathyroidism are three indicators: increased levels of parathyroid hormone and decreased or normal levels of calcium in the blood plasma, increased levels of phosphorus. The simultaneous detection of these three laboratory signs in a patient leaves virtually no doubt about the diagnosis of secondary hyperparathyroidism. Thus, with the classic bright variants of the course of the disease, its laboratory diagnosis cannot but amaze with its simplicity.
They learned to determine calcium in the blood a little over a hundred years ago - in 1907. In the blood, calcium is found in three main forms: the ionized fraction of the element - 50%, the fraction associated with proteins - 40-45%, the fraction consisting of complex phosphate and citrate connections - 5%. The main clinical laboratory parameters for studying this element in the body are the concentration of total calcium and the concentration of ionized (or free) blood calcium.
The range of normal values for total calcium in dogs is 2.25-2.85 and cats - 2.0-2.7 mmol/l; ionized calcium in dogs - 1.26-1.50 and cats -1.10-1.30 mmol/l.
In addition to its diagnostic value (to confirm the diagnosis of secondary hyperparathyroidism), the level of phosphorus in the blood serves as a differentiating criterion for distinguishing between primary (hyperfunction of the parathyroid gland, usually due to its degeneration) and secondary hyperparathyroidism caused by malnutrition during the period of intensive growth of the animal or chronic renal failure. In the second case, phosphorus levels tend to increase depending on the severity of renal dysfunction, which is associated with a loss of the ability to actively excrete phosphates. In addition to hyperphosphatemia, a distinctive feature of secondary hyperparathyroidism will always be a normal or reduced level of calcium in the blood.
The range of normal phosphorus values in dogs is 1.1-2.0 up to 6 months. – 0.9-2.1 and cats – 1.0-2.3 up to 6 months. 2.1-2.8 mmol/l;
Useful for diagnosing and establishing the severity of the disease are indicators of increased reorganization of bone matter and osteoresorption under the influence of prolonged excessive release of parathyroid hormone into the blood. Markers of osteoresorption include increased levels of alkaline phosphatase (its bone fraction). However, this indicator can increase in any form of hyperparathyroidism and other conditions associated with active restructuring of bone matter. Its values are more informative as indicators of the severity of damage to the skeletal system.
INSTRUMENTAL DIAGNOSTICS
X-ray research methods for secondary hyperparathyroidism include survey X-rays of the chest, abdominal cavity (allowing incidental detection of consolidated rib fractures, establishing spinal curvatures), as well as targeted X-ray examination of skeletal bones (diffuse thinning of the cortical bone, decreased bone density, hypertrophy of the periosteum, traces consolidated pathological fractures of the limbs, subperiosteal fractures, pronounced osteodystrophic changes in the skeleton).
The figures below illustrate these most common pathological changes in bones.
Secondary hyperparathyroidism can also occur in older cats as a result of chronic renal failure.
Increased activity of the parathyroid gland is a compensatory reaction of the body to hypocalcemia induced by meat foods or low calcium levels in the diet. The predominantly meat type of diet does not satisfy the cat’s body’s needs for microelements, primarily calcium, which is necessary for the normal growth of the animal.
This disorder occurs during periods of intense growth in young animals, as they require large amounts of calcium for growth and development.
TREATMENT
Treatment should be carried out by a specialist.
Treatment of patients with nutritional secondary hyperparathyroidism should be aimed at the main cause - normalization of the diet in terms of mineral composition.
Cage restriction to prevent bone fractures in animals with severe disease.
Laboratory studies and radiographs at intervals determined by your veterinarian are helpful in assessing improvement and response to therapy.
The purpose of monitoring is to track the dynamics of restoration of impaired functions (primarily the state of the skeleton), and to ensure that calcium metabolism indicators are normalized.
Animals without severe bone deformities have a good prognosis. Bone mineralization returns to normal within two to three months.
Disease in kittens and methods of treatment
The disease very rarely affects kittens, but the disease also occurs in babies. This happens, to a greater extent, due to the fact that the kitten is fed milk and dairy products, trying to replace the mother's milk with them. But this is a big mistake, which sometimes costs the kitten’s health.
Treatment of kittens also includes:
- proper, balanced nutrition;
- limited mobility (you can make a kind of playpen for him);
- drug treatment and vitamin supplements.
Prevention of eclampsia in cats
- A responsible owner must know the health status of his cat, therefore, together with a veterinary specialist, it is necessary to prepare the animal for pregnancy (clinical examination, laboratory diagnostics, etc.).
- Monitoring the diet based on the content of calcium, phosphorus, and minerals.
If the cat has previously been exposed to the disease, then the following is necessary:
- monitoring the animal during the entire period of bearing and feeding kittens by a veterinarian;
- long breaks between births.
Feline eclampsia is a dangerous disease that requires immediate treatment and further prevention throughout the animal’s life.
Preventive actions
What can (and should) be done to prevent eclampsia in cats? If your cat gave birth for the first time, and the disease struck her immediately after birth, it is better not to risk it: consult a veterinarian who will prescribe special calcium supplements to maintain normal levels of this substance in the blood. The entire time the cat is breastfeeding the kittens, she should be under the supervision of a veterinarian. These measures will not only help prevent recurrent cases of eclampsia! Such actions have a positive impact on the health of both the mother and her offspring.
Subacute therapy and maintenance treatment for chronic diseases
Supplementation of elemental calcium is given orally (Table 4) to ensure sufficient absorption of calcium in the intestine after the activating effect of vitamin D metabolites. Oral calcium is prescribed in the form of tablets or suspensions and plays the most important role in the initial period of treatment, especially if the animal has anorexia .
| Table 4. Treatment of hypocalcemia with oral calcium salts* | ||||
| A drug | % calcium content | Form | Dose (mg/kg per day) | A comment |
| Calcium carbonate | 40 | Pills | 25-50 | The most common calcium supplements |
| Calcium lactate | 13 | 325-, 650-mg tablets | 25-50 | |
| Calcium chloride | 27 | Powder | 25-50 | May cause stomach irritation |
| Calcium gluconate | 10 | Pills | 25-50 | |
| * When administering calcium orally, the dose should be calculated based on the content of basic calcium. | ||||
The mechanisms of active movement of calcium introduced into the intestine with low intake are under the control of calcitriol, and in the case of high calcium intake, passive absorption of calcium in the intestine occurs, independent of vitamin D. It is possible to take advantage of passive mechanisms to move calcium into the intestines before vitamin D takes effect there. Adequate foods contain sufficient amounts of calcium to maintain adequate calcium levels during treatment with vitamin D metabolites in many patients. Consequently, oral intake of calcium salts can in many cases be reduced and discontinued when the use of vitamin D metabolites reaches its maximum effect.
Of the calcium salts, calcium carbonate is the most widely used orally because it contains the largest percentage of basic calcium and this amount of calcium is contained in small tablets. The degree of calcium ionization and its biological value during absorption depend on the specific calcium salt and conditions inside the intestine; Therefore, it is not at all easy to determine the essential calcium content of a particular oral salt. Oral calcium is usually prescribed at a dosage of 25-50 mg/kg of basal calcium per day, divided into several doses. Oral calcium carbonate acts as a phosphate binder in the intestine in addition to providing additional calcium for intestinal absorption. It is advisable to continue treatment with oral calcium carbonate due to its phosphate-binding action in the intestine if serum phosphorus levels remain elevated. A decrease in serum phosphorus concentration leads to an increase in endogenous calcitriol synthesis due to attenuation of phosphate-mediated inhibition of the renal tubular la-hydroxylase system in the renal tubules.
Vitamin D preparations include ergocalciferol, cholecalciferol, dihydrotachysterol, 25(OH)-cholecalciferol (calcidiol), 1a-hydroxycholecalciferol, and 1,25-dihydroxycholecalciferol (Table 5). Ergocalciferol, dihydrotachysterol and calcitriol are most often used in veterinary medicine. Patients with primary hypoparathyroidism or persistent postoperative hypocalcemia require long-term treatment with some forms of vitamin D metabolites.
| Table 5. Treatment of hypocalcemia with vitamin D metabolites | |||
| A drug | Daily dose | Time until maximum action occurs | Time to eliminate the toxic effect |
| Vitamin D2 (ergocalciferol) | Initial - 4000-6000 units/kg per day Maintenance: 1000-2000 units/kg from 1 time per day to 1 time per week | 5-21 days | 1-18 weeks |
| Dihydrotachysterol | Initial: 0.02-0.03 mg/kg per day Maintenance: 0.01-0.02 mg/kg per ten. 24-48 hours | 1-7 days | 1-3 weeks |
| 1,25-dihydroxyvitamin D3 (calcitriol) | Initial: 20-30 ng/kg per day x 3-4 days Maintenance: 5-15 ng/kg per day | 1-4 days | 2-7 days |
Ergocalciferol is preferred by some due to its low cost, but it has several qualities that make it the least attractive of all calcium supplements. Ergocalciferol and its immediate metabolite 25-hydroxyergocalciferol have the lowest receptor avidity (the degree of affinity of antibodies to the antigen) of vitamin D, and therefore, to enhance the interaction with these receptors, high doses of the drug are required. Calcitriol is approximately 1000 times more potent than its source vitamin D and 500 times more potent at binding to natural calcitriol receptors than its predecessor calcidiol (25-hydroxyvitamin D). Ergocalciferol is highly soluble in fat, and it takes weeks to achieve the maximum effect of replenishing the body's reserves; It also takes a long time for it to be eliminated from the body. Therefore, after an overdose of ergocalciferol, prolonged hypocalcemia occurs. In addition, there is significant individual variation in the doses of ergocalciferol required to achieve the required serum calcium levels. Loading doses reduce the time required for maximum calcium action (see Table 3).
Dihydrotachysterol (DHT) is a synthetic analogue of vitamin D, and its maximum effect as a calcium supplement lies between that of ergocalciferol and calcitriol, as well as its half-life from the body. DHT has both 1a- and 25-hydroxy groups (after 25-hydroxylation in the liver), but lacks the 3-hydroxyl, which greatly reduces the effectiveness of 25-hydroxydihydrotachysterol in binding receptors. The polarity and low dosage requirements of DHT limit its storage in fat compared to ergocalciferol. Toxicity from hypercalcemia may be long-lasting (up to 30 days). Some patients require widely varying doses to achieve adequate calcium levels. Loading doses of DHT also tend to decrease the time for calcium to peak effect.
Calcitriol is a variant metabolite of vitamin D that has calcium effects due to the fastest onset of maximum effect and the shortest half-life in the body. The dose of calcitriol can be adjusted more often due to its more “real” effect on serum calcium. If hypercalcemia occurs, it is possible to quickly reduce the subsequent dose. The half-life of calcitriol in the blood is 4-6 hours, while its biological half-life is 3 to 4 days, which facilitates rapid resolution of hypercalcemia should it occur. There have been no reports of calcium loading doses using calcitriol in animals, but its use seems logical when more rapid correction of calcium levels is needed. The recommended dosage of calcitriol was 30-60 ng/kg per day; this dose may be satisfactory as a loading dose, but in our experience the OIA is too high for maintenance therapy in chronic cases. Doses of calcitriol in these cases range from 10 to 40 ng/kg per day, with an average dose of 10-20 ng/kg per day, divided in half throughout the day. We have used loading doses of 20-30 ng/kg per day for the first 3-4 days and maintenance doses of 5-15 ng/kg per day in many patients. The dose of calcitriol was divided in half daily to provide a supportive effect on the intestinal epithelium for calcium movement.
Calcitriol (Rocaltrol, Hoffmati-LaRoche), is commercially available in 0.25- and 0.50-mg capsules (250 and 500 ng per capsule, respectively). It is likely that calcitriol may need to be reformulated in doses to suit different animal sizes. It may be helpful to prescribe calcitriol in liquid form so that the dosage can be more accurately adjusted. Many pharmaceutical companies reformulate human drugs for veterinary purposes and create whatever dosage of calcitriol is needed.
When treating people with primary hypoparathyroidism, thiazide diuretics are sometimes used to reduce hypercalciuria. These drugs are especially helpful for people whose hypercalciuria continues even though their serum calcium levels are at the lower end of the normal range. Once thiazides are started, further reductions in the dose of vitamin D metabolites may be necessary as calcium levels increase due to renal calcium regeneration. The effect of thiazide diuretics on urinary calcium excretion is controversial in dogs and unknown in cats.
What not to do?
- In cats, vitamin D, necessary for this disease, is not synthesized in the body. An animal can only get it from food. Therefore, there is no need to irradiate the animal with a quartz lamp and expose it to the sun.
- You should not give or inject painkillers. If the animal stops feeling pain, it can aggravate its situation with even greater fractures.
It should be understood that this is almost always a curable disease, or at least one that can be kept within limits and prevented from progressing.
Treatment of subacute hypocalcemia
An initial bolus of elemental calcium usually reduces signs of hypocalcemia for a limited time (at least 1 hour and at most 12 hours) if the original cause of hypocalcemia remains. Vitamin D metabolites should be started as soon as possible, as they require at least a few days to maximally accelerate calcium transfer in the intestines. Supplementation with parenteral calcium salts is necessary to maintain adequate calcium levels until treatment with vitamin D metabolites remains effective in maintaining serum calcium within acceptable levels.
Multiple intermittent intravenous injections of calcium salts can be given to control clinical signs, but this method is not recommended because large fluctuations in serum calcium concentrations may occur. The remaining two options are continuous administration of calcium salts or their intermediate subcutaneous injection.
For continuous intravenous calcium administration, the recommended dose is 60-90 mg/kg basal calcium per day (2.5-3.75 mg/kg per hour) until the required calcium level can be achieved with oral medications. Initial doses in the higher range are given to patients with more severe hypocalcemia, and then the dose is reduced according to the calcium level achieved. The dose of intravenous calcium is also reduced in the future as calcium salts and vitamin D taken orally become more effective.
10 ml of 10% calcium gluconate solution contains 93 mg of basic calcium. A convenient method of administering calcium is to administer an intravenous solution in a volume of 60 ml/kg per day (2.5 ml/kg per hour). Approximately 1 mg/kg per hour, 2 mg/kg/hour and 3 mg/kg per hour of basal calcium are provided by adding 10, 20 and 30 ml of 10% calcium gluconate solution, respectively, to each 250 ml liquid bottle. Apparently, the same degree of calcium delivery can be achieved by adding 20, 40 or 60 ml of 10% calcium gluconate solution to each 500 ml liquid bottle to administer the desired dose.
Calcium salts should not be added to liquid medicinal preparations that contain lactate, acetate, bicarbonate and phosphate, as the calcium salts may precipitate. Treatment with alkalinizing fluids containing sodium bicarbonate reduces the amount of ionized calcium and produces clinical signs of hypocalcemia in animals with borderline hypocalcemia and should therefore not be used.
Options for subcutaneous administration of solutions containing calcium are possible. Calcium gluconate should be diluted before subcutaneous injection in a ratio of at least 1:1; Calcium chloride should not be used as it causes severe tissue irritation. An initial dose of calcium to combat tetany can be given 3-4 times a day or a dose of 60-90 mg/kg divided and administered subcutaneously several times a day. Doses for subcutaneous calcium administration should be reduced as with continuous calcium administration.
Symptoms
What are the symptoms of osteoporosis in cats? In the initial stages, you will not see anything specific. But when the course of the disease worsens, the clinical picture becomes characteristic. Firstly, stupid fractures that happen literally at every step. Secondly, sick animals may constantly experience constant pain, although they do not have any visible injuries. This is caused by microcracks in the bones, causing a powerful pain reaction. It is known that some people with osteoporosis had their necks literally “on their word of honor”, so deep were the cracks in the vertebrae!
Diagnosis of hyperparathyroidism
To make an accurate diagnosis, a visual examination of the pet is carried out and a conversation with the owner about the animal’s behavior and diet. An unbalanced diet is evidenced by the constant consumption of milk porridge, baby meat puree, fatty meat and low-quality industrial feed. If the diet is incorrect, the kitten does not receive all the necessary minerals and the required amount of phosphorus and calcium.
To confirm hyperparathyroidism in a cat, an X-ray examination is performed. With endocrine disease, the following can be clearly visible on an x-ray: low bone density, curvature of the spine, pathological mini-fractures and tail breaks. After confirming an accurate diagnosis, a course of treatment is prescribed depending on the age of the pet, the course of the disease and the condition of the sick animal.
To establish an accurate clinical picture of the disease, laboratory tests are prescribed to determine the hormonal state of the parathyroid gland and the level of phosphorus and calcium ions in the blood. Laboratory tests, radiography, examination and consultation with the animal owner allow us to determine an accurate diagnosis and prescribe appropriate treatment.
Prevention
If this disease has bypassed your pet, this does not mean that it will not appear in the future. But we can do everything necessary to protect our pet because the disease is easier to prevent!
- Balanced feeding, with the correct ratio of phosphorus and calcium, will ensure the animal a long and healthy life.
- Regular visits to the veterinarian will help identify and neutralize the disease at the earliest stages.
Main causes of feline hyperparathyroidism
The main cause of the disease, which is indicated by all veterinarians without exception, is improper nutrition of the pet. Unfortunately, not all owners carefully select the diet for their ward. According to experts, the best diet for kittens will be one that contains approximately the same amount of phosphorus and calcium.
However, most dry foods provide animals with approximately 20-25 times more phosphorus than calcium. In this case, systemic changes occur in the cat’s body: trying to ensure a sufficient amount of calcium in the blood, parathyroid hormone begins to “suck” this trace element from the bone tissue and supply it to the blood system.
The natural system of the cat’s body tries to cope with the problem on its own and instead of bone tissue in the animal’s skeleton, fibrous tissue is grown. The situation worsens when kittens often eat foods such as fish, cereals, and meat. They all contain a lot of phosphorus.
Secondary hyperparathyroidism has slightly different reasons for its development. In addition to the lack of calcium in food, there is insufficient absorption of the microelement by the kitten’s digestive system. This happens with various pathologies of the digestive system, diseases of the thyroid gland, liver failure, excess magnesium and vitamin D. Sometimes hyperparathyroidism can develop if the animal grows too quickly.
Main causes of the disease, diagnosis
- Poor nutrition during pregnancy and the postpartum period.
- Inconsistency of the calcium-phosphorus ratio with the physiological needs of the animal.
- Gastrointestinal diseases that interfere with the normal absorption of these substances.
- The pathology most often occurs in first-born cats, since the body of young cats has not yet had time to properly adapt.
How can a veterinarian make the correct diagnosis? In many ways, everything depends on you, since you will have to provide the specialist with the maximum information he needs. Once again, we warn you that you need to immediately tell your doctor about your pet’s pregnancy or recent birth, as this is the most important sign indicating illness. After all, it’s not called “postpartum eclampsia in cats” for nothing.
It will be necessary to conduct a routine blood test and its biochemical study. If it turns out that the calcium concentration is less than 18 mol/liter, then your cat definitely has eclampsia. It is important to remember that with this pathological condition, low levels of sugar and magnesium in the blood are often detected. In addition, a serological study in this case reveals that the potassium content in the serum is sharply increased. Of course, the ECG will show pathological contractions of the cardiac striated muscles.
Treatment of acute hypocalcemia accompanied by tetany or seizures
Tetany or seizures caused by hypocalcemia require treatment with calcium salts administered intravenously. The effective dose of calcium is 5-15 mg/kg of basic calcium (0.5-1.5 ml/kg of 10% calcium gluconate solution) over 10-20 minutes. The percentage of calcium in the preparation varies widely and depends on the specific calcium salt (Table 3). There is no difference in the effectiveness of intravenous calcium salts in reversing hypocalcemia if the dose is based on basal calcium levels. Calcium gluconate is often used as a calcium salt, since it does not cause irritation if its solution gets outside the vessel; calcium chloride causes severe tissue irritation, but contains more basic calcium per milliliter of solution (see Table 3).
| Table 3. Treatment of hypocalcemia with parenteral calcium* | ||||
| A drug | Preparation | Calcium concentration | Dose | A comment |
| Calcium gluconate | 10% solution | 9.3 mg calcium/ml | Slow acting IV (0.5-1.5 ml/kg) Recommended 5-15 mg/kg per hour IV Recommended 1-2 ml/kg in a 1:1 ratio with saline solution subcutaneously three times a day | Discontinue if bradycardia or QT interval shortening Infusion to maintain normal calcium levels May be given subcutaneously |
| Calcium chloride | 10% solution | 27.2 mg calcium/ml | 5-15 mg/kg per hour IV | Only IV, because has a strong irritant effect on tissue |
| * Do not mix calcium solution with bicarbonate-containing solutions, as precipitation may occur. | ||||
During urgent administration of calcium salts, it is necessary to monitor the heart rate and electrocardiogram. Bradycardia serves as a signal of the onset of cardiotoxicity due to too rapid administration of calcium; A sudden increase in segment threshold, shortening of the QT interval, or premature ventricular complexes also indicate cardiotoxicity from calcium administration. Not all clinical signs will immediately disappear after urgent correction of hypocalcemia; the elimination of some of them is delayed for 30-60 minutes. Nervousness, shortness of breath, and changes in behavior may remain despite calcium normalization during this period; possibly reflecting a delay in equalization of calcium levels between the cerebrospinal and extracellular fluids (as this process occurs slowly). It will also take some time for the hyperthermia caused by the increased activity of muscle tremors to resolve.
Etiology: why does hyperparathyroidism develop?
In a healthy pet, the ratio of calcium to phosphorus in the body should be the same. If the owner does not monitor the diet of the growing kitten, then he has an excess or deficiency of these substances, as a result of which hypercalcemia or hyperparathyroidism is diagnosed. The primary form of bone disease in kittens can occur due to hyperplasia of the parathyroid glands and is known as hyperparathyroidism. As a result of the disease, the amount of parathyroid hormone increases. Secondary nutritional hyperparathyroidism develops due to poor absorption of calcium. This phenomenon occurs due to impaired functioning of the gastrointestinal tract or thyroid gland.
Veterinarians note that calcium deficiency is associated with rapid growth of the kitten.
Description
There are 2 forms of hyperparathyroidism:
- Primary - characterized by increased levels of parathyroid hormones. The disease occurs due to dysfunction of the gland itself. This form of pathology is very rare. Typically, primary hyperparathyroidism is diagnosed in older cats with parathyroid hyperplasia or enlarging tumors.
- The secondary form is the most common. Its development is caused by kidney disease, in which the balance of electrolytes in the body is disturbed. As a result, the amount of phosphorus increases and the level of calcium in the blood decreases. To correct the imbalance, the body begins to intensively produce parathyroid hormone. Against the background of such disorders, there is a decrease in the level of calcitrol, which is the active form of vitamin D. It is produced in the kidneys and helps improve the absorption of calcium from the intestines. Its deficiency in the body leads to disruption of the process of bone mineralization.
A nutritional form of hyperparathyroidism, caused by excess phosphorus in the diet, is common in kittens. For normal formation of bone tissue, the ratio of calcium and phosphorus in the skeleton and blood must be constant.
An imbalance occurs as a result of the kitten's intake of predominantly meat food, which is rich in phosphorus but contains little calcium. A cat is a predatory animal that, under natural conditions, eats its prey along with the bones, thus replenishing its body with calcium. Pet owners often feed them beef, chicken, liver, and sausage. Introducing cottage cheese and milk into the diet does not save the situation, since the level of phosphorus in dairy products is 2 times higher than the amount of calcium.
Kittens are susceptible to the disease due to the fact that the growing body requires tens of times more calcium compared to an adult. Most often, Maine Coons, Siamese, British and Scottish kittens suffer from hyperparathyroidism.
The progression of the disease leads to the formation of multiple pathological bone fractures - both folded and microfractures, which are not visible on x-rays. Damage to the pelvic bones causes severe deformation of the pelvis and disruption of the bowel movement. Fractures or cracks in the spine cause neurological disorders.
Diagnostic procedures
If such an illness is suspected, the furry puppy should see a doctor as soon as possible. The sooner owners detect hyperparathyroidism in kittens and contact a veterinary clinic, the higher the chances of a favorable outcome and prevention of many complications. The specialist must clarify the pet’s diet and conduct a visual inspection. To detect hypoparathyroidism, your veterinarian will order x-rays for cats. If the symptoms of the disease appear due to dysfunction of the endocrine system, then the kitten’s bones in the pictures are almost transparent, the spinal column is curved and several small fractures are observed. After diagnosis, the specialist will tell you how and how much to treat the cat. The selection of a therapeutic course is influenced not only by the degree of hyperparathyroidism, but also by the age of the kitten and its general condition.
How to identify hyperparathyroidism
To accurately diagnose pathology, it is best to use x-rays. Tests will not show reliable levels of trace elements in the blood. In most cases, the results will be normal.
In turn, an x-ray will immediately show that bone density has decreased; some bones may look transparent or thinned. There will be less contrast between soft tissue and bone. The image will also show undetected fractures that have already healed or were not noticed before the examination.
X-rays can also evaluate bone deformation. To study the development of the disease in question, you will need to examine the pelvis and chest.
If neurological disorders are present, the condition of the spine is additionally assessed. In severe situations, curvature of the vertebrae, overcrowding of the intestines or bladder can be determined. These pets need urgent help.